Hemorrhagic
1
View details
A 48-year-old man presents to the emergency department with a profuse nosebleed from the right nostril that began spontaneously 45 minutes ago. He reports attempting to pinch his nose at home for 15 minutes without success. This is his third episode of severe epistaxis this week, though the previous two resolved with compression. He reports a long history of recurrent nosebleeds since his teenage years, which have increased in frequency and severity over the last decade. He endorses feeling fatigued recently and notes shortness of breath upon climbing two flights of stairs. He denies any recent facial trauma, upper respiratory infection, or intranasal drug use. He is not currently taking anticoagulants or antiplatelet medications.
His family history is significant for his father requiring multiple blood transfusions for "chronic nose issues" and a stroke at age 60. The patient has no known allergies.
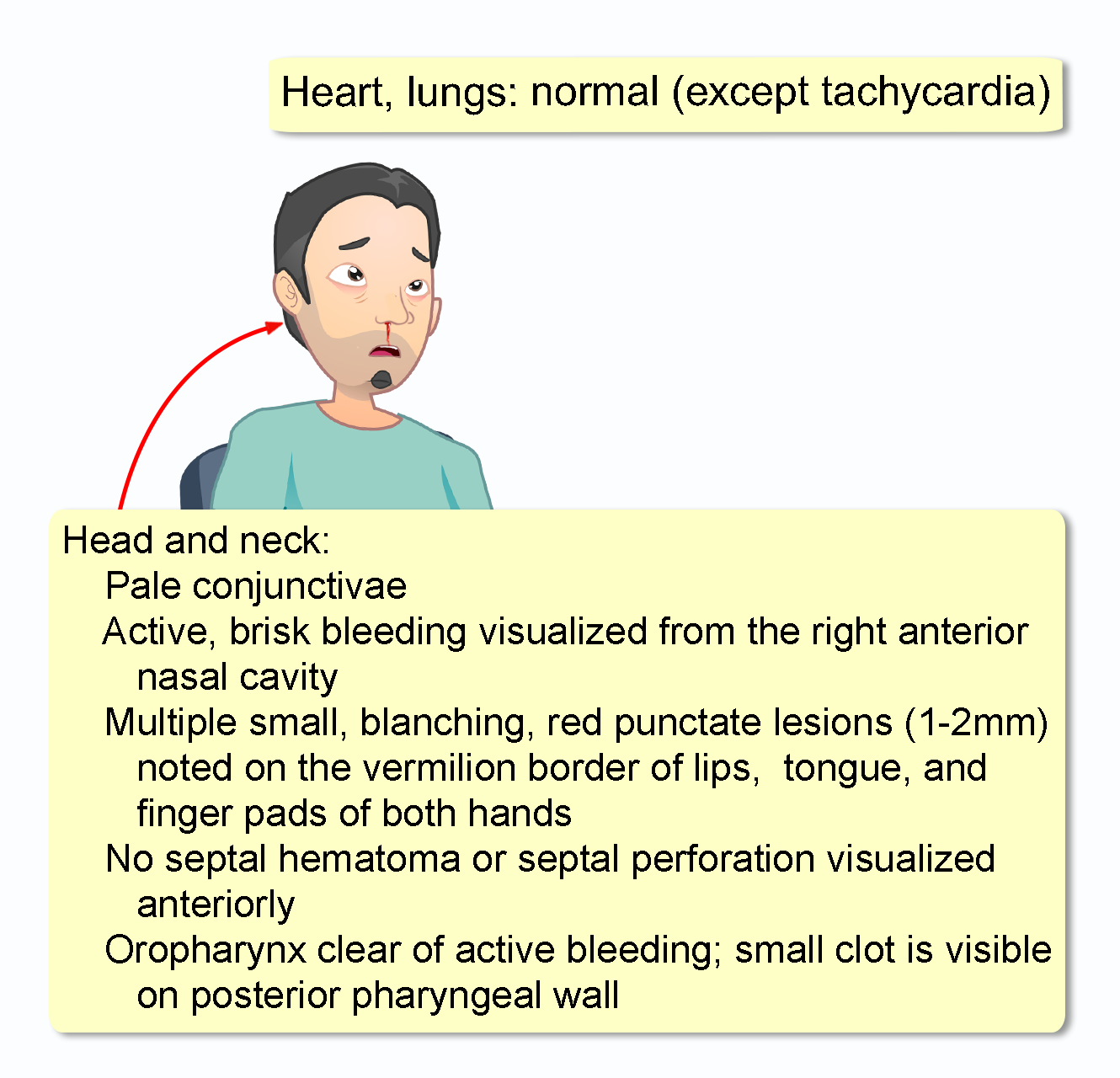
His temperature is 98.6o F (37o C), pulse is 105 bpm, respirations are 18/min, blood pressure is 138/84 mm Hg, and O2 saturation is 98% on room air. He is alert and anxious appearing, and he holds a blood-soaked towel to his face.
Initial laboratory results obtained upon arrival are as follows:
WBC: 7,500/mm3 (4,500-11,000)
Hemoglobin: 9.8 g/dL (13.5-17.5)
Hematocrit: 30% (41-53)
Platelets: 245,000/mm3 (150,000-400,000)